At a glance:
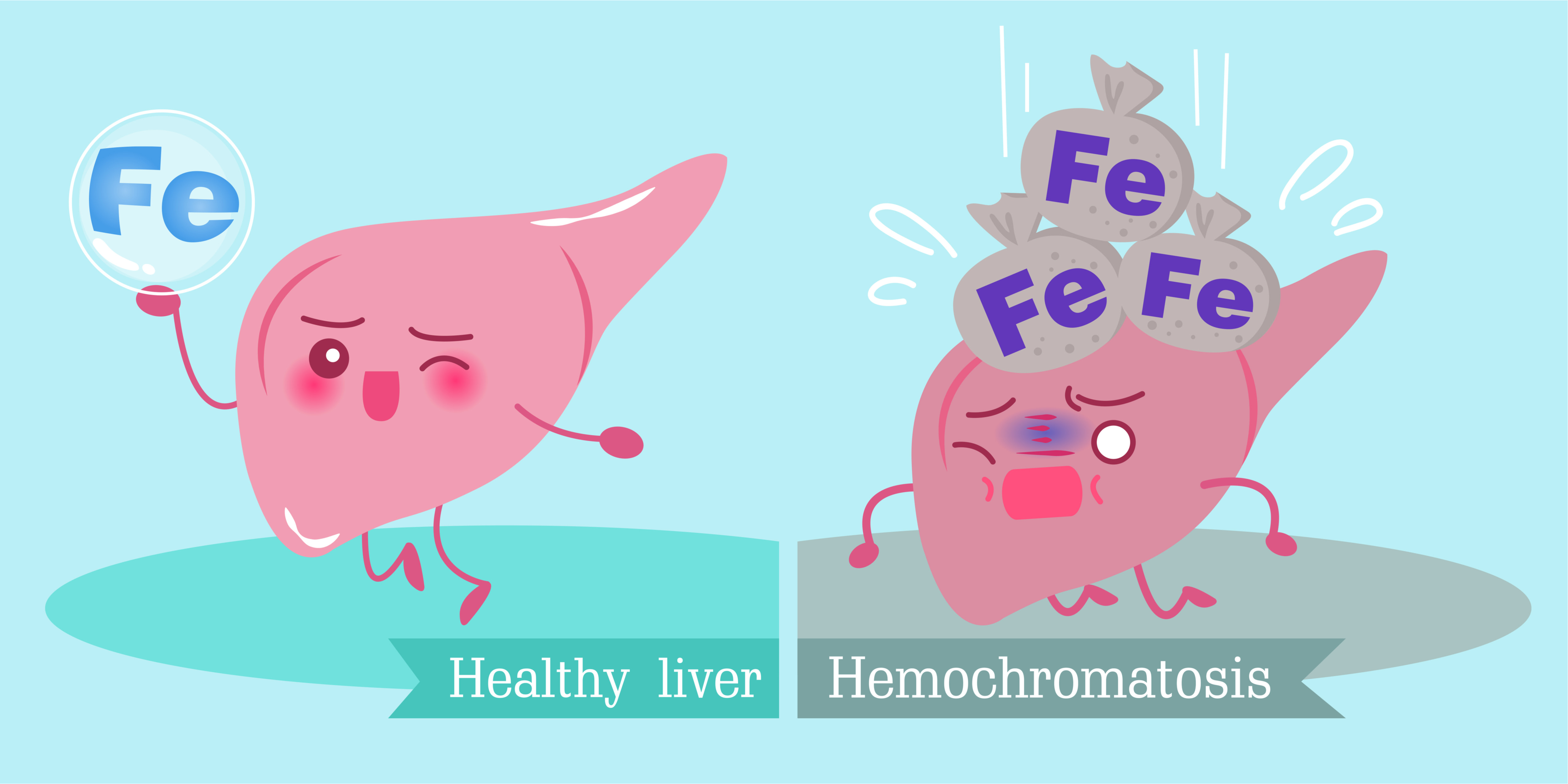
- Haemochromatosis is a condition that causes the body to absorb excessive iron.
- Around one in 200 Caucasians carry the genes that may develop into haemochromatosis.
- Iron is necessary for carrying oxygen around the body, but the amount in the body is carefully regulated.
- When too much iron is absorbed it is deposited in organs and joints.
- The body has no way to excrete iron so the deposits build over time potentially leading to organ damage and a wide array of symptoms.
- Haemochromatosis may be difficult to diagnose due to the symptoms being common to a wide variety of conditions.
- The condition can’t be cured but is manageable through venesection (regular blood removal) as well as changes to diet and lifestyle.
What is Haemochromatosis?
Not having enough iron in your body may lead to a number of adverse effects, but did you know that having too much iron in your body may be just as dangerous?
Haemochromatosis (Iron Overload Disorder) causes people to absorb excessive iron from their diet and is a relatively common genetic disorder in Australia. Around one in 200 people of northern European descent (Causasians) have genetic risk factors for haemochromatosis that may lead to the development of the disease.
In a normal person, the majority of the iron in the body is found in haemoglobin (a protein in red blood cells) with any extra being stored in the liver. This stored iron is used when iron in the body is depleted. The body has no mechanism for excreting excess iron, so the body controls iron levels by only absorbing the amount it needs from food.
The body typically has one gram or less of iron stored, but in a person with haemochromatosis, the body doesn’t stop absorbing iron at that limit and instead keeps building the stores of the trace mineral. Excess iron is stored in the joints and organs and as the body has no way to excrete the stored iron it continues to build up over time.
Organs such as the liver, heart, pancreas, brain & hormonal glands may be damaged by the excess stored iron, and iron in the joints may lead to arthritis and other joint problems. Both men and women, particularly between the ages of 30 and 60 are at risk of developing haemochromatosis. Women tend to develop the condition later in life than men as regular menstruation may help deplete excess iron.
Although it is common, Haemochromatosis is also under-diagnosed, in part because the symptoms of the condition are common to a number of other health issues.
Symptoms of Haemochromatosis
No two people with haemochromatosis share the exact same symptoms and for some the condition may be asymptomatic. Symptoms, if there are any, develop slowly over time as iron builds up in the organs or joints and may not be noticed until the symptoms become severe.
This slow development of symptoms combined with the fact that many of them are shared by numerous other conditions or the effects of aging may make haemochromatosis difficult to diagnose.
If your doctor suspects haemochromatosis they may schedule a number of tests to determine the amount of iron in your blood. If the blood test returns abnormal results, further testing, such as genetic testing, an MRI scan to detect the amount of iron in the liver, or a liver biopsy may be needed to complete a diagnosis.
Common symptoms of haemochromatosis include:
- Fatigue - weakness and lethargy.
- Joint Issues - from joint pain to arthritis and osteoporosis.
- Abdominal Pain
- Diabetes - excess iron buildup in the pancreas may lead to problems with insulin production and diabetes.
- Liver Disorders - excess iron in the liver may lead to a swollen liver, cirrhosis (scarring), liver disease or even liver cancer.
- Sexual Disorders - in women, excess iron may affect ovarian tissue leading to irregular, abnormal or even absent periods loss of sex drive or premature menopause. In men, iron overload may lead to erectile dysfunction, reduced libido and gynecomastia (the swelling of breast tissue).
- Skin Disorders - the skin may turn “bronze” or tan. A person with hemochromatosis may also lose body hair.
- Heart Disorders - iron deposits in the heart may lead to heart rhythm problems and muscle damage (cardiomyopathy)
- Neurological Disorders - iron overload may lead to issues with memory.
- Psychological/Mood Disorders - including depression, mood swings, impulsiveness or anger problems.
- Weight Loss - as with most symptoms of haemochromatosis, weight loss may take some time so may not be overly noticeable.
- Hypothyroidism - iron overload may affect the thyroid gland leading to an underactive thyroid.
If you have a family history of haemochromatosis, or have been experiencing a wide range of symptoms, schedule an appointment with a doctor to see if you have an abnormal HFE gene.
What Causes Haemochromatosis?
Haemochromatosis is a genetic disorder and, as such, anyone carrying the abnormal genes may develop the condition. Genetic screening may be used to identify if someone has the gene responsible for haemochromatosis.
HFE, the gene responsible for hereditary haemochromatosis is autosomal recessive. This means that for the gene to be passed on both the mother and father must have the abnormal HFE genes. Approximately one in seven people have a HFE mutations making them potential carriers capable of passing on the gene to children. Carriers will not develop haemochromatosis themselves, only carry a gene that may be passed on.
In addition to having the gene, there appear to be a number of factors that may increase the chance of developing haemochromatosis, including:
- Age - iron builds up over time so is more likely to be found in higher quantities in older people.
- Alcohol - drinking alcohol with meals may increase iron absorption as well as stress an already overtaxed liver.
- Dietary Iron - eating iron rich food or drinking water with high levels of iron.
- Iron Supplements - consuming too many iron supplements or eating iron enriched food (such as cereals).
- Vitamin C - vitamin C aids in the absorption of iron.
Blood loss through injury or donation, blood transfusions, and various forms of anaemia may also affect the chance of someone developing haemochromatosis.
Treatment for and Living With Haemochromatosis
As the condition affects the way in which the body absorbs iron, treatment and management of the condition revolves around both removing excess iron from the body as well as limiting iron intake.
One of the key treatments for haemochromatosis is known as venesection or phlebotomy. During venesection, blood is removed (in a manner similar to blood donation) helping to reduce iron levels. When new blood is being produced, iron is needed to build haemoglobin and the body draws from the stored deposits in the liver and other areas.
Depending on the severity of the case and how early it has been detected, early stages of venesection may require the person with haemochromatosis to have around 500ml of blood taken on a weekly or even twice weekly basis for an extended period of time (around 18 months). Once the levels of iron are in an acceptable range, the frequency of venesection may be reduced to monthly, quarterly or less.
Venesection may be performed in a number of different practices, such as your GP or most hospitals. The Australian Red Cross Lifeblood also offers therapeutic venesection services..
Dietary and lifestyle changes are also necessary to ensure that iron intake is limited. Such changes may include:
- Limiting the amount of iron rich food that is consumed (red meat, offal, iron enriched foods, etc).
- Reducing the amount of alcohol consumed. People with liver damage due to haemochromatosis should avoid alcohol altogether.
- Avoiding vitamin C and iron supplements.
Dietary changes should be discussed with a doctor before they are adopted.
The easiest and most convenient way to make medical appointments is to search and book online with MyHealth1st.